When the Body Won’t Let Go
There’s a reason why some people say they “carry stress in their hips.” Beneath your abdominal organs, running deep alongside your spine, lies a powerful muscle that silently records your body’s history of safety and threat — the psoas.
Often overlooked in both medicine and mental health, the psoas is more than a hip flexor. It’s a messenger between your body and your brain, your movement and your emotions, your past and your present. When life keeps you braced for impact — from ongoing stress, burnout, or unresolved trauma — the psoas often becomes one of the first places to tighten, shorten, and hold on.
Understanding the psoas could be the missing piece in your journey to healing. It’s not just about flexibility or posture — it’s about safety, survival, and learning to soften again.
What Is the Psoas?
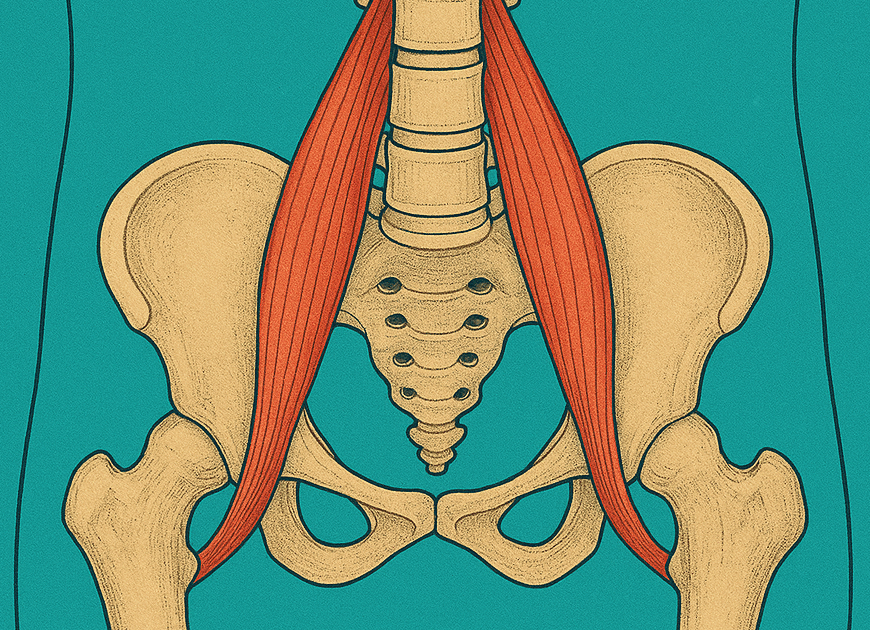
The psoas major is a deep-seated muscle that runs from the lumbar spine to the top of your thigh bone (femur). Together with the iliacus, it’s often called the iliopsoas. This muscle group helps lift your leg, stabilize your spine, and support your posture.
But the psoas also lives in the neighborhood of your nervous system, diaphragm, and internal organs. Its proximity to these vital structures means it doesn’t just move your body; it listens to your internal state. It responds when you’re scared. It tenses when you’re bracing. And it remembers when you felt unsafe.
Its location means it interacts constantly with the autonomic nervous system (ANS). The ANS is responsible for involuntary functions like heart rate, digestion, and respiration. More importantly, it regulates your responses to perceived danger through the sympathetic (fight or flight) and parasympathetic (rest and digest) branches. The psoas becomes activated when the sympathetic nervous system is triggered — essentially bracing you for danger. But when that danger is no longer present and the psoas can remain contracted, which means the nervous system doesn’t get the memo that it’s safe again.
The psoas is sometimes called the “muscle of fear” because it is directly wired into how the body expresses fear.
Why the Psoas Reacts to Stress
The psoas is hardwired into your survival system. When your brain detects a threat, whether it’s physical, emotional, or even perceived (such as social rejection or performance anxiety), it activates the hypothalamic-pituitary-adrenal (HPA) axis. This cascade releases cortisol and adrenaline, preparing the body to respond.
The psoas contracts to prepare you to run, jump, or protect your core. This is an elegant survival strategy. But the body is not built for constant activation. If the nervous system remains on high alert due to chronic stress, unresolved trauma, or ongoing environmental pressures, the psoas doesn’t get a chance to soften.
This chronic contraction turns into physical tension, postural changes, and emotional exhaustion. Over time, the line between body memory and emotional state blurs. You might not remember the original event, but your psoas does.
Signs Your Psoas Is Holding On
A chronically contracted psoas can quietly shape your physical and emotional well-being. Common signs include:
-
-
- Persistent tightness or discomfort in the hips or lower back
- Shallow breathing or a sense that you “can’t take a full breath”
- Restlessness, anxiety, or difficulty relaxing
- Fatigue or postural imbalances
- Digestive issues or pelvic discomfort
-
Research in somatic psychology and trauma therapy has shown that the body encodes stress as patterns of muscular holding. According to Dr. Bessel van der Kolk, author of The Body Keeps the Score, trauma reshapes both the body and the brain, specifically the limbic system. The psoas becomes part of that reshaping.
The Feedback Loop Between Body and Brain
When the psoas remains tight, it continues to send signals of danger to the brain. The brain, in turn, activates more sympathetic nervous system responses: increased heart rate, reduced digestion, heightened alertness. This creates a loop:
Tight psoas → increased sensory signals of danger → brain interprets tension as ongoing threat → sympathetic nervous system re-activates and releases more stress hormones → more psoas tension → parasympathetic (rest-and-digest) functions decrease
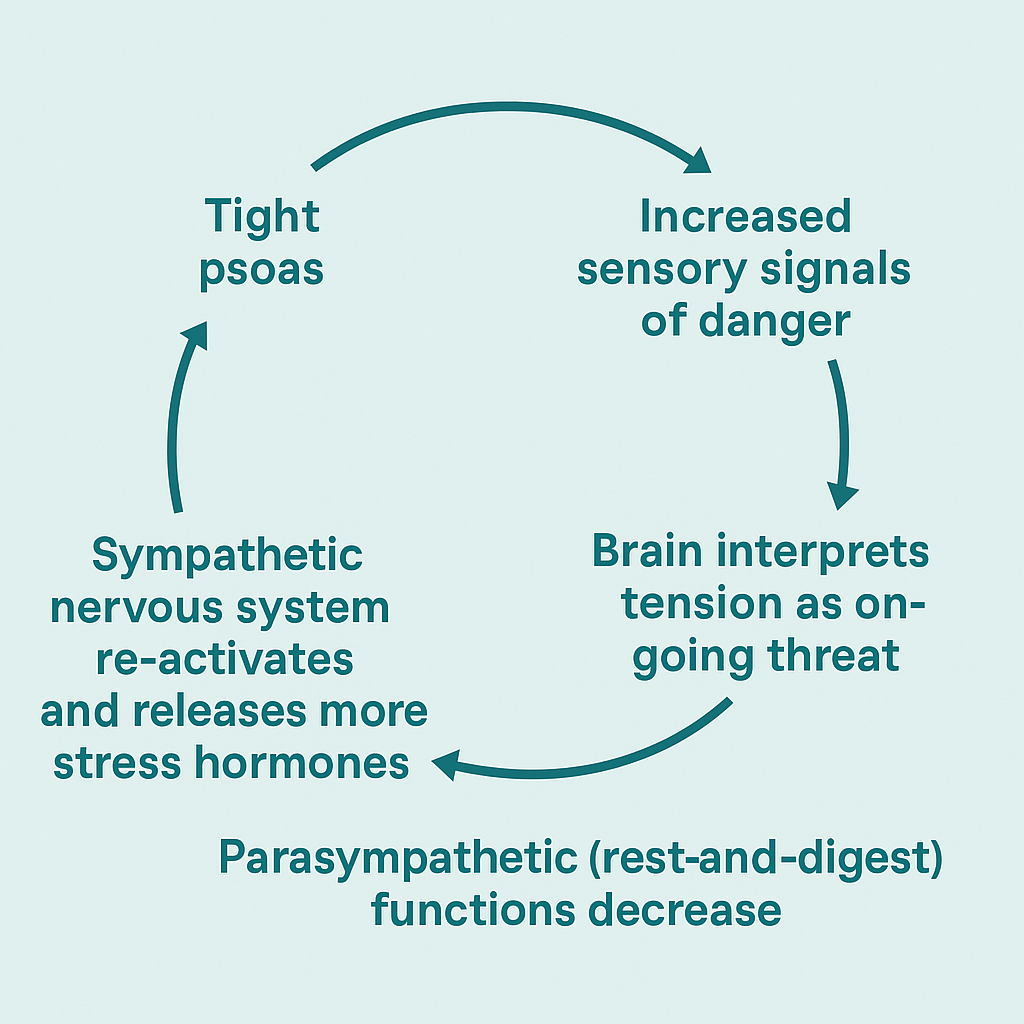
This loop doesn’t just affect the muscles. It impacts your ability to regulate emotion, sleep deeply, or feel safe in relationships. In bottom-up therapy, we start with these physical responses to help interrupt the loop.
The Psoas and the Diaphragm: Partners in Breath and Safety
The diaphragm (your main breathing muscle) and the psoas are connected by fascia and share attachments along the spine. When the psoas is tight, it can restrict the diaphragm’s movement, leading to shallow breathing.
This relationship is key to understanding why trauma survivors often describe a feeling of breathlessness. It’s not just anxiety, it’s a physical compression that limits how deeply they can breathe. Without full breath, the vagus nerve (which calms the body) can’t do its job as effectively.
The vagus nerve is a major player in the parasympathetic nervous system. When stimulated by slow, diaphragmatic breathing, it sends calming signals throughout the body. But if the psoas is rigid, it limits this breath-induced regulation. This is one reason why nervous system healing must include bodywork, breath, and trauma-informed movement.
Why the Psoas Is Called the “Muscle of the Soul”
Yogis and somatic therapists have long referred to the psoas as the “muscle of the soul.” While this might sound poetic, it speaks to the deep, emotional resonance of this muscle. The psoas doesn’t just react to stress — it stores it. It holds the body’s silent stories of fear, freeze, and flight.
Studies in polyvagal theory, introduced by Dr. Stephen Porges, suggest that our physiological state dictates our capacity for social engagement, emotion regulation, and even cognition. If the psoas is on constant alert, you may find yourself stuck in a chronic “protective” state, unable to access curiosity, openness, or connection.
A New Path to Healing
Understanding the psoas opens the door to a different kind of healing. One that doesn’t start with changing your thoughts, but with listening to your body. If your psoas is still on guard, your nervous system may still believe the world isn’t safe.
When you’re ready, we’re here to walk with you. Learn more about our body-based therapy services and how they can begin to tell the psoas a new story: one of support, release, and real safety.
Get Matched with a Therapist.
Because finding support should never be as hard as what you’re going through.