What Your Hips Might Be Trying to Tell You
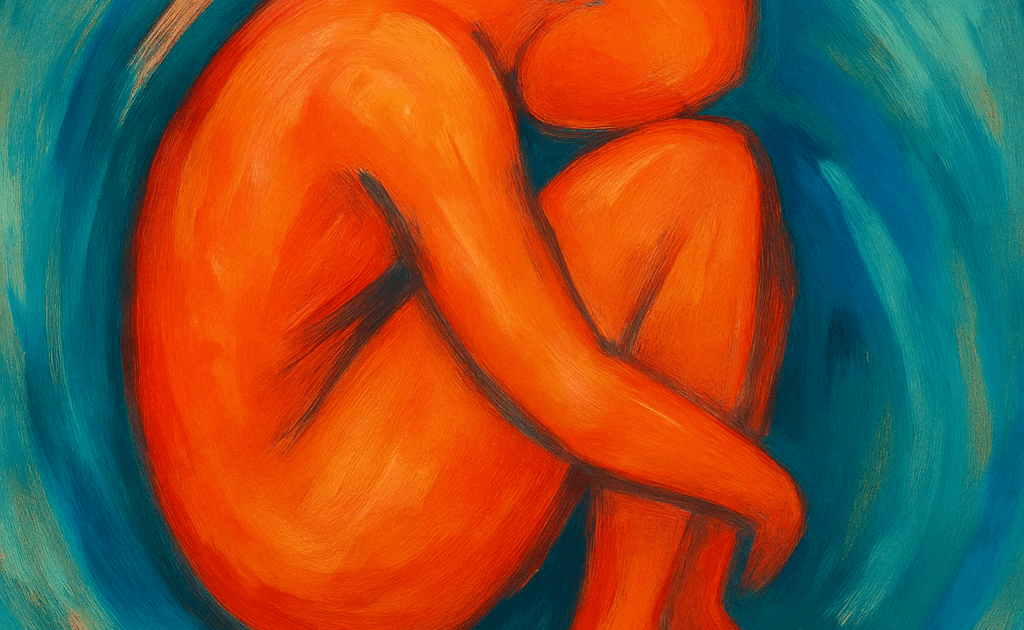
Ever tried to stretch out your hips only to feel like nothing changes? You’re not alone. The psoas muscle, nestled deep within your pelvis, doesn’t always respond to traditional stretching. That’s because what it’s holding isn’t just physical tension — it’s protection. And true release requires more than movement. It requires a felt sense of safety.
The Psoas Muscle: More Than Just a Hip Flexor
Tucked deep within your core, the psoas connects your spine to your legs. It’s essential for movement — helping you walk, sit, stand, and stabilize your posture. But its role doesn’t stop there. Because of its proximity to your diaphragm, spine, and nervous system, the psoas also plays a powerful role in how your body responds to stress and fear.
It’s no wonder, then, that the psoas is often called the “muscle of fear.” Not because fear lives inside it — but because it’s wired directly into how your body expresses it.
Why Stretching Alone Falls Short
The psoas is a survival muscle. It doesn’t operate on willpower or effort. If your nervous system doesn’t feel safe, the psoas won’t release — no matter how long or deeply you stretch.
This is because it’s part of your body’s protective reflex — the same system that kicks in when you brace for impact. It holds a form of implicit memory: your body’s stored record of times it had to tense in order to survive. Neuroscience shows that trauma lives in the subcortical brain — areas like the brainstem, limbic system, and basal ganglia. These aren’t influenced by logic or language. They respond to cues of safety.
The psoas doesn’t need to be pushed — it needs to feel safe enough to soften.
Start with Safety: The Felt Sense Comes First
In trauma-informed therapy, we focus on creating felt safety — not just the intellectual knowing that you’re okay, but the physical and emotional experience of it.
That’s why we begin with practices like:
-
-
- Grounding: Lie on your back with knees bent and feet flat. Feel your body sink into the support beneath you. Let gravity do the work. Imagine your energy settling downward like roots growing into the earth.
- Orienting: Slowly look around your space. Land your eyes on something that feels calming or neutral. Let your body register: “Right here, right now, there’s no danger.”
- Co-regulation: Spend time with a therapist or someone whose calm presence helps your system settle. Safety is often something we first borrow from another nervous system.
-
These practices help activate the parasympathetic nervous system — your body’s “rest-and-digest” state. And when that happens, the psoas gets the message: it’s safe to let go.
Breathwork: The Psoas-Calming Prescription
Your diaphragm and psoas are intimately connected — physically and neurologically. They’re neighbors in the body, wrapped in shared fascia, and they communicate constantly. When the diaphragm moves freely, it encourages the psoas to soften too.
Here’s a simple breathing exercise to try:
-
-
- Inhale slowly through your nose for 4 counts
- Exhale gently through your mouth for 6–8 counts
- Rest one hand on your belly and one on your chest. Invite your breath to drop low.
-
This kind of breathing increases vagal tone, improving your nervous system’s ability to regulate stress. It’s also deeply linked to better digestion, mood, and immune response. Think of each breath as a quiet message to your psoas: you’re safe now.
Gentle Movements that Re-Educate, Not Force
Instead of stretching with intensity, we use mindful movement to invite the body into a new experience:
-
-
- Pelvic tilts: Rock your pelvis gently while lying on the floor — forward, back, and side to side.
- Supported lunges: Use props or cushions so you can rest in the posture without strain.
- Hip circles: Move the hips in slow, exploratory circles from a seated or tabletop position.
-
Each motion is paired with breath and curiosity. The goal is not to fix, but to rebuild relationship and safety. This is neuroplasticity in action — your nervous system learning that softness is possible.
You can’t force safety into the body, but you can create the conditions for it to return.
Therapies That Support Psoas Release
Several body-based approaches help unwind psoas tension by working with the nervous system, not against it:
-
-
- Somatic Psychotherapy: Supports the body in completing protective responses it never finished.
- IFS (Internal Family Systems): Addresses inner parts that hold fear or control.
- EMDR: Helps the brain reprocess traumatic memories so the body doesn’t stay braced.
- Breathwork: Uses conscious breathing to create space in the body and calm the system.
- Body LENS Neurofeedback: Helps regulate the brain and vagus nerve, supporting deep internal balance.
- Trauma-Informed Yoga: Offers safe, guided movement that gently lengthens the psoas over time.
-
All these modalities access the parts of the brain where trauma lives — allowing your body to move from freeze to flow.
Releasing Isn’t the Goal. Trust Is.
Psoas release isn’t something you force — it’s something that happens when your body finally believes it no longer has to protect you.
This is the heart of bottom-up healing: we don’t start with changing thoughts, we start with changing signals. When the body begins to feel safe, everything else can follow — mood, memory, connection, even posture.
True healing doesn’t happen by pushing. It happens by restoring trust.
A Gentle Invitation
If your body is still holding on, there’s nothing wrong with you. It just hasn’t felt safe enough to let go — yet. When you’re ready, reach out to us. Explore our somatic therapy services and learn how reconnecting with your body can be the first step toward lasting relief.
Get Matched with a Therapist.
Because finding support should never be as hard as what you’re going through.