How to Recognize the Signs, Understand Post Traumatic Stress Responses, and Find the Right Help
There is a quiet kind of suffering that often hides in plain sight. It doesn’t always announce itself with flashbacks or nightmares. Sometimes it shows up as chronic self-doubt, intense shame, or the inability to feel safe when there’s no danger. For many, this isn’t just post-traumatic stress—it’s complex PTSD.
If you’ve ever felt like you should be “over it” by now, but you’re still stuck in patterns that don’t make sense, you’re not alone. Your nervous system isn’t broken. It adapted. And there’s a way forward.
What Is PTSD & How Is It Different from Complex PTSD?
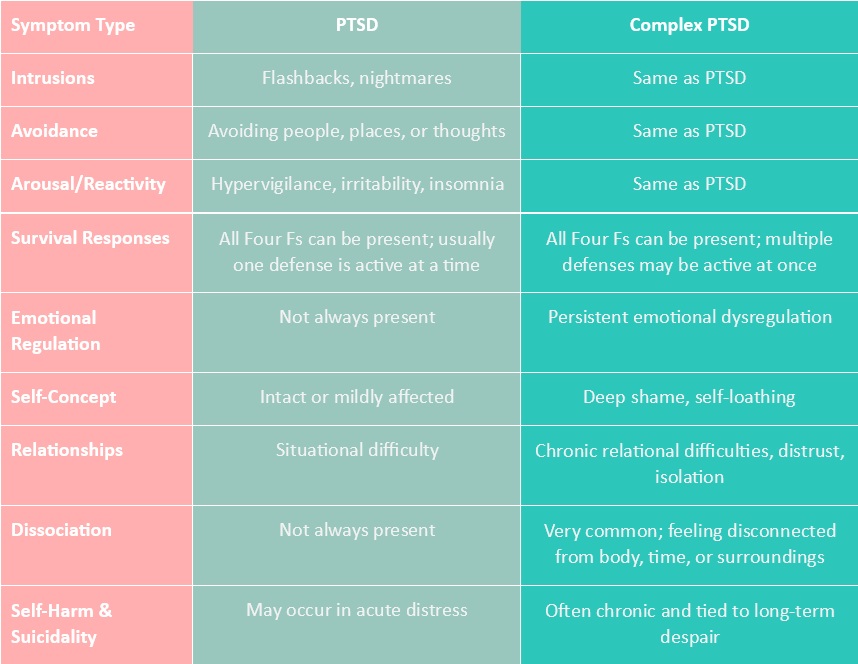
PTSD typically develops after a single, intense traumatic event—a difficult loss or accident, an assault or robbery, a life-threatening situation etc… Symptoms often include flashbacks, avoidance, emotional numbing, hypervigilance, and intrusive thoughts.
Complex PTSD (also known as CPTSD), on the other hand, stems from prolonged, repeated trauma—often in early development or relationships. Think ongoing abuse, neglect, or unsafe caregiving environments. CPTSD includes all core PTSD symptoms but adds deeper struggles with emotional regulation, a persistent sense of worthlessness or shame, and difficulty in relationships.
Here’s one way to imagine the difference: PTSD is like a lightning strike that scorches a single area, while CPTSD is more like a slow-moving wildfire that reshapes the entire landscape. In CPTSD, the brain’s network—its emotional wiring and cognitive assumptions—are fear-based by default. The world doesn’t just seem unsafe; it is unsafe, because that was the only reality your system knew. Survival becomes the default setting.
These patterns often show up as the Four F’s—Fight, Flight, Freeze, and Fawn. They’re not failures. They’re the body’s best attempts at safety:
-
-
- Fight: Anger, defensiveness, control to manage threat
- Flight: Anxiety, overworking, perfectionism to stay ahead of danger
- Freeze: Disconnection, paralysis, dissociation when escape feels impossible
- Fawn: People-pleasing, appeasing, merging with others to reduce threat
-
How PTSD Affects the Brain?
Trauma reshapes how the brain functions. Not metaphorically—literally. These changes aren’t about weakness or lack of effort; they’re survival strategies carved into the brain itself:
-
-
- Amygdala (fear center): Acts like an overly sensitive alarm system. After trauma, it gets stuck on high alert, constantly scanning for danger even when none is present. Everyday stressors may feel life-threatening.
- Hippocampus (memory & context): Functions like a faulty recall system. It can shrink in response to chronic stress, making it hard to separate past from present. This is why traumatic memories can feel like they’re happening all over again.
- Prefrontal Cortex (executive function): Works like the brain’s braking system. Under trauma, this area goes offline, making it harder to regulate emotions, think clearly, or hit the brakes on reactive behavior.
- Stress Hormones: Cortisol and adrenaline act like the body’s fuel injectors. When they’re constantly released, they can wear the system down, contributing to inflammation, poor sleep, digestive problems, and chronic pain.
-
When all these systems are dysregulated, it can feel like you’re driving with a jammed accelerator (amygdala), faulty memory GPS (hippocampus), and no working brakes (prefrontal cortex).
This is why healing can’t be done through CBT reasoning or positive thinking alone. Trauma lives in the body—and healing has to meet it there.
When trauma hits, your brain becomes a car in crisis—alarms blaring (amygdala), GPS glitching (hippocampus), brakes misfiring (prefrontal cortex), and the fuel pedal stuck down (stress hormones).
Relational Impact: Why Living with Complex PTSD Hurts Connections
When your nervous system is wired for survival, connection can feel like a risk. Even when you want closeness, your body may be bracing for betrayal, abandonment, or engulfment.
-
-
- You may crave love but feel unsafe when it’s offered.
- You may shut down, withdraw, or become overwhelmed by emotional intimacy.
- You may feel intensely responsible for others’ feelings (fawn), or cut people off when things feel too intense (flight or freeze).
-
These reactions are not who you are—they’re what your nervous system learned. CPTSD often makes people feel “too much” or “not enough” in relationships. But at its root, it’s a story of safety strategies trying to protect a deeply relational being.
Can PTSD Be Cured?
Trauma doesn’t vanish overnight. But the brain is plastic—meaning it can rewire.
Through consistent, well-matched care, the amygdala can learn that it’s safe to relax. The prefrontal cortex can strengthen. New pathways form, new beliefs take hold. This is neuroplasticity in action. It doesn’t erase the past, but it builds a present that feels more manageable, more connected, and more yours.
Healing is not about “going back to normal.” It’s about building a new normal—one rooted in safety, self-compassion, and real connection.
For people with Complex PTSD, the therapeutic relationship itself becomes a powerful part of recovery.
How to Find the Right Help for PTSD and Complex PTSD
Finding the right therapist isn’t just a logistical step—it’s one of the most important parts of healing from complex trauma.
For people with CPTSD, the therapeutic relationship itself becomes a powerful part of recovery. Research consistently shows that the quality of the connection between client and therapist is one of the strongest predictors of successful outcomes—especially for trauma. Why? Because CPTSD is, at its core, relational trauma. It stems from repeated experiences where connection was unsafe, inconsistent, or unavailable.
This means that therapy isn’t just about processing memories or learning tools. It’s about having a relationship where safety, consistency, and trust can begin to grow.
When seeking a therapist for PTSD recovery, look for someone who:
-
-
- Specializes in trauma and nervous system regulation
- Works slowly and collaboratively, attuning to your pace and readiness
- Uses modalities like IFS, EMDR, somatic therapy, mindfulness, and DBR
- May refer or collaborate with naturopaths or integrative practitioners
- May offer neurofeedback or collaborate with others for deeper regulation and rewiring when needed
-
At Inner Summits, we know that finding the right fit can feel overwhelming—especially if you’ve had past experiences where you felt misunderstood or unsafe. That’s why we offer a guided therapist matching process. You don’t have to tell your story over and over again or navigate the search alone. Our founders take the time to get to know your needs, preferences, and history to help match you with a therapist who feels like the right fit from the start.
CPTSD recovery isn’t a one-size-fits-all treatment plan. At Inner Summits, we offer integrative, bottom-up approaches that meet your nervous system where it is:
-
-
- Somatic Therapy: Works with body awareness and nervous system regulation
- IFS (Internal Family Systems): Helps parts of you feel seen, heard, and healed
- EMDR: Reprocesses traumatic memories while supporting nervous system balance
- Neurofeedback: Calms brainwave patterns and supports emotional regulation
- Mindfulness: Anchors attention and creates pause between reaction and response
-
Other helpful supports include:
-
-
- Expressive Arts Therapies: Art, movement, music as outlets for emotional release
- Yoga & Breathwork: Restore connection between mind and body
- Naturopathic Medicine: Supports sleep, hormones, and inflammation through holistic care
-
Closing Thoughts on PTSD vs. Complex PTSD
If any of this resonated, know this: there is nothing wrong with you. Your system adapted to survive what it lived through. And now, it deserves to feel safe.
You are not alone. There is a way forward. And when you’re ready, we’re here to walk with you. Call us for a free consultation with one of our founders.
Get Matched with a Therapist.
Because finding support should never be as hard as what you’re going through.